SIBO and Stress: 3 Ways Your Nervous System Keeps Your Gut Stuck
You finished your SIBO eradication protocol. Your retest is clear. You did the work and yet you are still bloated, constipated and reacting to foods. If that sounds familiar, you are not alone. One reason we see all the time in the clinic, and it is often overlooked, is the link between SIBO and stress. Not just the feeling of being stressed, but what stress does to the nervous system and how that changes digestion and motility.
You have probably heard someone say, “just reduce your stress and your gut will heal.” It’s a nice idea, but it is not that simple. Stress is one piece of the puzzle. It influences whether your gut can switch back into rest-and-digest, whether motility turns on and whether the small intestine stays clear after SIBO has been addressed.
Last Updated: November 2025 by Bella Lindemann
In this blog we will work through:
Part 1: Stress can block SIBO protocols from working
When you are stressed, your body shifts into fight or flight mode. In that state survival gets priority and digestion gets pushed to the background. Blood flow leaves the digestive tract. Stomach acid, bile and enzyme production fall. Gut motility, or the way your gut moves food along, starts to shut down.
The biggest casualty is the migrating motor complex, or MMC. Think of the MMC as your small intestine’s clean up crew. Between meals, rhythmic waves move food particles, bacteria, archaea and waste along the small intestine. This cleansing wave keeps the small intestine clear. It is essential for preventing SIBO, bloating, constipation and other symptoms.
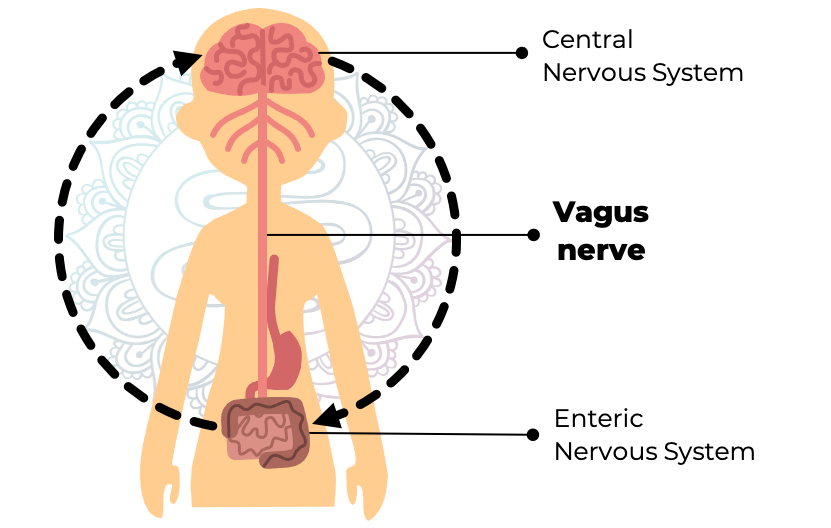
The MMC is controlled by the enteric nervous system and it is strongly influenced by the vagus nerve. The vagus nerve is the main line of communication between your brain and your gut. When you’re in stress mode and feeling anxious, overworking, undersleeping or constantly tense, your vagus nerve tone weakens. When vagal tone is low, MMC cleansing waves don’t run properly. That means the clean up does not happen and debris and microbes sit longer than they should in the small intestine.
“Even if you’re taking the right SIBO antimicrobial supplements to eradicate the overgrowth, and following your protocol perfectly, if motility isn’t functioning properly, bacteria and archaea can hang around and symptoms won’t go away.”
One way I like to explain it is this: You can have a clean kitchen, but if everyone is stressed and no one is doing the dishes, the mess builds up fast. That is what a suppressed MMC looks like. It’s one reason why your SIBO protocol might not work properly if your vagus nerve, and nervous system as a whole, isn’t supported.
Part 2: Stress can cause SIBO to relapse
Now imagine you completed your protocol. Your retesting is clear. Things feel better for a while, then out of nowhere the old symptoms creep back. The reason is often the same mechanism. The MMC does not just help during eradication, it protects you between meals and overnight by clearing the small intestine and keeping microbes at the right levels and where they belong.
If vagal tone stays low, those cleansing waves do not sweep through. Food and microbes can linger in the small intestine and backflow from the large intestine into the small intestine (through the ileocecal valve) has an easier path to follow. Over time conditions tip toward overgrowth again. You can be eating well and taking prokinetics, yet if your nervous system still signals ‘not safe’ motility will not keep pace and relapse risk rises.
This is why nervous system support isn’t optional, it’s a core part of relapse prevention in our clinic. We layer it into protocols as a non-negotiable, the same way we would layer in meal spacing, digestive supports, prokinetics and microbiome rebuilding.
Part 3: Symptoms can remain even when SIBO is gone
This is the part that frustrates people the most. Your breath test is clear, your stool test looks better, yet you still feel puffy and uncomfortable and react to foods, or have other lingering SIBO symptoms.
In many cases, the overgrowth has been addressed but digestion has not fully switched back on. The vagus nerve is still quiet. The MMC is still underperforming. The body is still carrying a stress load, so rest-and-digest is not the default.
When we look deeper, we often see patterns like these on functional testing and tracking devices:
High cortisol or a flipped cortisol curve on a DUTCH hormone test
Signs of sluggish motility on a GI-MAP stool test, along with other markers that point to low digestive secretions
Low heart rate variability trends and other signs of nervous system dysregulation in the person’s day to day life.
Until your body shifts into a true rest-and-digest state, your gut won’t function optimally. You may continue to have bloating, altered transit time, food sensitivities, constipation or diarrhea.The internal environment is not calm enough to run normal digestive programs. This is where the vagus nerve matters.
The vagus nerve is your gut’s on switch
The vagus nerve is like a remote control for digestion. It’s what shifts your body into parasympathetic mode, or ‘rest and digest’, where healing, repair and proper gut function happen. Healthy vagal tone supports stomach acid release, bile flow and enzyme production, motility and the MMC, and it also helps to regulate immune activity in the gut lining.
When vagal tone is strong, digestion can flow smoothly. When vagal tone is weak, things slow down and symptoms appear. The hopeful part is that you can train vagal tone with simple targeted daily practices. You do not need an hour a day, you only need a few minutes, done consistently.
Five daily gut calming habits we use with clients
These are the nervous system supporting tools we give to almost all of our clients who are recovering from SIBO or other gut dysfunction. They are simple and they work when you do them regularly.
1. Deep belly breathing before meals
Spend a few minutes breathing slowly into your belly before you eat. This helps flip your body into rest-and-digest mode. It primes stomach acid and enzyme release and sets up the MMC to do its job between meals.
2. Humming or gargling
Two to four minutes a day is enough to stimulate the vagus nerve through your vocal cords and throat. It may feel silly, but it's surprisingly effective. We often ask clients to do this in the shower because who doesn’t love to hum along to a catchy tune when the acoustics are good?
3. Gentle movement
Walking, yoga and stretching support motility without pushing cortisol and triggering a stress response in the body. If you are already burnt out, high intensity sessions can make symptoms worse. We often keep clients in the gentle zone until sleep and energy improve.
4. A brain dump journal
Often the stressor is not the schedule, it is the constant mental load that keeps your nervous system stuck in fight-or-flight. Take five minutes in the morning or evening to write down your thoughts or to-do list. Getting it on paper tells your brain it is handled and that signals safety to your body.
5. Prioritize sleep
Aim for seven to nine hours of quality sleep each night. Poor sleep raises cortisol, weakens immune function and suppresses the MMC. If you struggle with sleep, focus on a wind-down routine, dim the lights, reduce screen time before bed and keep your bedtime consistent. If you need even more support, magnesium glycinate can help if it is tolerated.
Start small and stay consistent. These are the habits that retrain the nervous system and support long term gut function.
Next steps: healing is possible
If your protocol has stalled, if your symptoms keep coming back, or if you have a clear SIBO retest but your gut still feels off, it may not be the food or the supplements. It may be your nervous system.
Stress doesn’t cause SIBO on its own. Stress can block your protocol from working, cause it to relapse, or keep symptoms lingering. That is why this piece is just as important as your antimicrobials, diet and other recommendations.
Support your vagus nerve daily. Give your body clear signals of safety. Build the simple habits that let digestion turn back on. This is how we help clients move from short term symptom relief to stable, long term gut health.
If you're ready to feel better, we’re here to help. You can:
Book an Initial Consultation with one of our experienced SIBO specialists and get started today.
Explore our recommended supplements through our Supplement Dispensary.
Or simply learn more about our process and how we work with clients via a Complimentary 15 Minute Pre-Consultation call with one of our practitioners.
About author: Bella Lindemann, FDN-P
Bella Lindemann is the founder and lead practitioner at The Functional Gut Health Clinic. With her science degree, functional nutrition certification and extensive experience, she is a recognized expert in gut health and the science of SIBO, parasites and other gut infections. With her own personal gut healing experience and having supported thousands of clients across the clinic, Bella is passionate about helping her clients address GI imbalances and take back control of their digestive symptoms.