Is a Gut Infection the Hidden Cause of Your IBS?
Have you ever followed a healing diet like Paleo, SCD, GAPS or low-FODMAP to control your IBS symptoms? You might have felt great for a while, and then found that your gut symptoms came creeping back. And you felt like a complete failure because these diets are supposed to control IBS, right!?! What if I told you that no matter how perfectly you stick to that diet it isn’t going to work on its own if a hidden gut infection is the root cause of your IBS.
Here is a summary of what we are going to cover:
> What is a gut infection?
> Factors that increase your risk of getting a gut infection
> What symptoms to look out for and why a hidden gut infection is often the cause of IBS
> The go-to tests I use with my clients and why a previous “clean” result might be misleading
> How to treat a gut infection and why many people fail
So often we have the same story
My story, like so many other chronic and autoimmune disease sufferers (whether they know it or not), started with a gut infection - food poisoning from a dodgy seafood buffet in Africa and four days chained to the toilet, to be precise. After a few courses of antibiotics and a diagnosis of food sensitivities to dairy, eggs and gluten (amongst others), things should have improved… but they didn’t. Well, they did initially, when I worked through every gut-healing diet known to man. But then came the long downward slide into chronic IBS and a whole host of secondary conditions like fatigue, weight gain and anxiety before finally falling off the cliff - cutting back my work days and avoiding social outings like the plague - almost five years after the original infection.
But, according to the many doctors I sought out along the way, there wasn’t anything seriously wrong. I just had IBS and needed to eat more fibre, drink more water and manage my stress. Oh, and use laxatives if I get really constipated. Maybe I should consider antidepressants? As if I wasn’t frustrated enough already, this “band-aid” strategy suggestion pushed me over the edge.
And so it is with the majority of my clients, many of whom have been well and truly put through the ringer by the opinions and diagnoses of other professionals. In fact, I get almost all of my clients with chronic G.I. issues or autoimmune conditions to properly test for gut infections and rarely see one come back clean. These can include parasites, bacteria and yeast infections or overgrowths, all of which are pretty common and often overlooked as the root cause of IBS.
What is a GUT INFECTION?
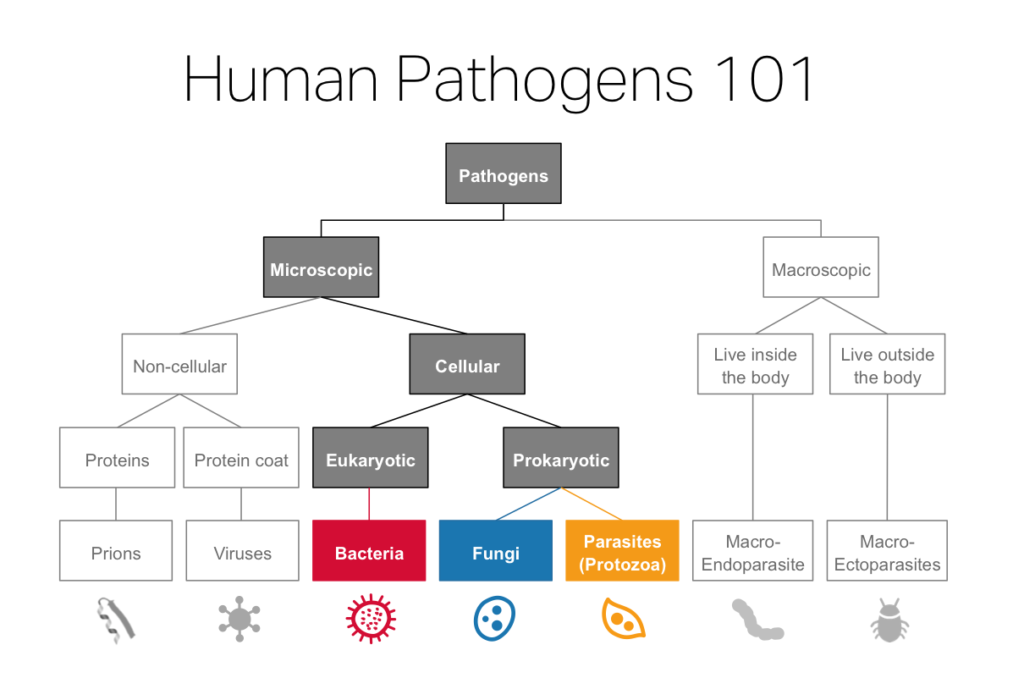
When I’m talking about gut infections, I’m referring to infections anywhere from the stomach right through to the small intestine and the colon. They are caused by pathogens, the most common being:
Parasites: Blastocystis hominis, Entamoeba histolytica, Giardia lamblia, Cryptosporidium parvum, Dientamoeba fragilis
Bacteria: Helicobacter pylori, Citrobacter, Campylobacter, Clostridium difficile, Klebsiella pneumoniae
Fungi/Yeast: Candida albicans
While this isn’t an exhaustive list of gut infections (see diagram below), Parasites, Bacteria and Fungi are by far the most common I see in my practice and the ones I specialise in treating.
What are the risk factors?
It’s not always travel that leads to a gut infection, but it is certainly one of the most common causes. Food poisoning, overly affectionate pets or an outbreak in your town’s water supply can all give you a nasty bug. You see, pathogens are a normal part of life in every country on earth, it’s whether your immune system is strong enough to fight it off that really matters.
It’s why we have stomach acid, good bacteria in our gut and an immune system to fight-off these ‘bad guys’ (1, 2). But, if you are stressed, intoxicated, fatigued, have food sensitivities or any other illness or condition, your immune system is likely to be compromised, increasing your risk of a gut infection with potentially lasting effects, like IBS (3, 4, 5).
Prior use of antibiotics (often used to kill another gut infection) is also a very common cause of gut infections, particularly Candida and SIBO (6). While antibiotics can sometimes be effective at killing the primary bacterial infection, by destroying all the good bacteria at the same time, they also create an environment for opportunistic pathogens and overgrowths to proliferate and cause long-term chronic conditions (7).
Why a Gut Infection is often the root cause of IBS?
Here are a couple of ways you can figure out if your IBS symptoms are being impacted by a gut infection:
> Cyclical diarrhea - most parasites have specific life cycles and result in cyclical symptoms, such as diarrhea. So, if you are doing ok for a week or two and then have an intense flare-up of symptoms for a few days and then do ok for another week or two and so on, that can be a real sign of a parasite.
> Constipation - pathogenic bacteria can give off neurotoxins to ‘paralyse’ the muscles around the intestines, slowing peristalsis (intestinal movement) so that the organisms don’t get removed by the stool as easily as they may have before. Constipation can then create an environment in which pathogens can further grow and proliferate (8, 9).
> Gas and bloating - gas results when bacteria ferment intestinal contents, commonly fermentable dietary fibre and carbohydrates. Small Intestinal Bacterial Overgrowth (SIBO) is a common example of this and why many people see reduced symptoms on a low-FODMAP diet which is low in fermentable foods (10).
> Reflux, heartburn or indigestion - some pathogens, like H.pylori, affect stomach acid production and our ability to digest foods properly, and can result in reflux, heartburn and indigestion-type symptoms (11, 12).
> Real food diet failures - if you have any IBS symptoms after you’ve tried any of the real food / low allergen diets like SCD, GAPS, Paleo or low-FODMAP diets for more than six weeks, then there is a high chance you have a gut infection.
> Secondary symptoms - like fatigue, hormone imbalances, weight gain, insomnia, anxiety and malabsorption from a Leaky Gut can all be the result of a gut infection (13, 14).
How to test for a gut infection
If you have any, or a combination, of the above symptoms and risk factors, you’re probably wondering how to figure out who might be hiding in your gut. There are three main tests I use:
1. Comprehensive Digestive Stool Analysis + PCR
A stool test is the oldest and most common form of testing for gut infections. While traditional techniques using visual (microscope) detection aren’t always reliable, the new approach using DNA sampling (PCR) is much improved (15, 16). This is why if you have had a stool test done by your GP in the past and it came back clean, this doesn’t mean there isn’t an infection. It might just mean the test you did didn’t detect it or wasn’t looking for the particular pathogen that you have.
The most common test I have my client’s complete from DSL is called a GI-MAP DNA Stool Analysis, which is a comprehensive assessment of the microbiological environment of the gut. It reports on pathogenic (parasites, bacteria and yeast/fungus) and imbalanced colonising organisms, as well as identifying the levels of beneficial flora. This is done using DNA detection, rather than the traditional visual microscopy approach, meaning it is much more accurate.
GI-MAP Stool Analysis Test Result - Example Extract
2. SIBO Breath Test
Small intestinal bacterial overgrowth (SIBO) is not a pathogen, but rather an overgrowth of commensal (normal) bacteria that grow in your large intestine that have now found a home in your small intestine (where they definitely don’t belong!) (17). Because there are no ‘bad guys’ to find, it is a condition that has largely gone undetected or undiagnosed until recently. Which explains why it accounts for up to 80% of IBS cases (that is, cases that have not previously found a causal agent for the gastrointestinal symptoms) (18). The current ‘gold standard’ of testing is the three-hour lactulose breath test for SIBO (19). It’s all a bit scientific, but basically, not all breath tests are created equal. The substance used (lactulose, glucose, etc), the byproduct being tested (CO2, hydrogen, methane, etc.), timing, number of samples and many other variables matter. I use the SIBO Basic Lactulose test by SIBO Test with my Australian clients.
SIBO Breath Test Result - Example Extract
3. Organic Acids, Intestinal Dysbiosis Panel
If the CDSA stool test comes back clean, the organic acids panel can be an alternative testing option, particularly for identifying yeast overgrowths such as Candida. This simple urine test measures the overflow or build-up of organic acid production in the urine, allowing us to detect imbalances in bacterial, yeast and fungal markers. There are a few labs that I use for this test such as the Microbial Organic Acids Test by The Great Plains Laboratory.
Great Plains Organic Acids Test Result - Example Extract
If you think this sounds like you, get in touch and we can do some testing to figure out what is going on in your gut: CLICK HERE.
It is also really important to understand the importance of relapse and retesting. Many treatments (particularly conventional ones like antibiotics) have a very short-term success rate. That is, they kill a pathogen and if you retest in 2 or 3 weeks it will not show-up. Retest 8, 12 or 16 weeks later and it’s likely back again… or did it really ever leave? You see, many bugs have various lifecycles that see it active or dormant, easy or hard to kill. And if you only take 10 days of antibiotics, chances are, you’re not going to do the job properly. So, after any protocol, we always wait a further 60 days before retesting to make sure we’ve got it for good.
How do I heal my gut infection?
Successfully healing a gut infection requires a holistic approach focussed on fixing the root cause of your problems and supporting your body through the healing process. This means we are going beyond just temporary symptom relief by supporting your body throughout the whole pathogen eradication protocol. That is, from being healthy enough to fight-off an infection right through to healing the body and making sure you are strong enough to fight-off any attempted reinfection or other opportunistic pathogens in the future.
Because every client and every gut infection is so individual, it’s impossible to give specific details in a blog post like this, but I’m keen to try to educate you on many of the considerations that go into developing a pathogen eradication protocol.
Treating gut infections can be hard work. Not only are the pathogens often difficult to kill, the impact on the rest of your body during the process can be draining. Every heard of “die-off”? It’s a real thing and it sucks. Basically, when the bugs die, they let off toxins that make us feel terrible (20). This is why it is really important to support your body, in the form of liver detoxing, rest, etc. while completing a pathogen eradication protocol.
One particular challenge that often arises is the case of multiple pathogens and the order in which to treat them. The simple rule is: 1st Parasite, 2nd Bacteria and 3rd Yeast. Why? Because parasites put out ‘bug-poop’ that will feed bacteria and yeast so they have to go first. Yeast feed off anything and are hugely opportunistic so they have to go last. When the environment is as healthy as we can get it the yeast can’t live there in abundance anymore and they move on out. That is a healthy gut microbiome!
Treatment Protocol
When it comes to eradicating and healing from a gut infection, I put my clients on a protocol that addresses diet, rest, exercise, stress reduction and supplementation. We specifically focus on the following:
Diet
Once we know what type of gut infection/s you have, we can choose a diet that works for you. The primary food sources for most gut infections are sugar and starch so these must go. The Specific Carbohydrate Diet (SCD) or a Paleo Diet can be a good place to start. For SIBO, I like to layer the low-FODMAP diet over these to remove some other short-chain carbohydrates.
The next thing we need to consider is removing your food sensitivities that cause inflammation and can damage your gut lining. These are identified by a food sensitivity test. Some fermented foods are allowed based on tolerance of the individual. Focus on organic products and aim for 2-3 litres of water (room temperature) or herbal tea to flush out toxins put out by the bugs as they die off.
Rest
Rest is an essential component of any healing protocol and often overlooked. Know this: if you don’t give your body the rest it needs to heal, you will not get better! Ideally, go to bed before 10pm. 7-8 hours sleep each night is an absolute must. Good “sleep hygiene” means turning off those screens (phone, laptop and TV) and allowing one hour before sleep each evening to wind-down by reading a book, journaling, meditating or listen to relaxing music. Trust me, this practice alone will change your quality of sleep if you commit.
Exercise
Too much or too intense exercise for those with a gut infection can put added stress on the body and do more harm than good. While it’s always important to move your body, a more gentle approach, with exercise such as walking, yoga and restorative pilates will likely have the most positive impact on your healing. Once your gut is in better shape, you can return to all of the crazy-active things you love. Read more about this HERE.
Stress Reduction
Removing and reducing stress on the body is a crucial part of any gut infection healing protocol. This applies to all three categories of stress:
Mental/emotional: implementing relaxation and stress reduction activities such as meditation or acupuncture
Physical: consider working with a chiropractor or other health professional to address any structural problems adding to your body’s overall stress
Hidden/internal: these are things like hormone imbalances, liver issues, food sensitivities or leaky gut that we need to test for and eliminate to stop the constant inflammation in your body. A gut infection itself is a hidden stressor and one that must go for you to return to full health.
Supplementation
Through my study and clinical practice, I have learnt that it is extremely challenging to completely eradicate a gut infection using diet alone. A pretty shocking truth and why we need to be smart and supplement, using natural botanicals - nature’s ultimate anti-pathogenic treatment.
A few of my go-to supplements to support the body and heal a gut infection include:
First line of defence:
Natural antimicrobial herbal blends - This is the product that will kill off the bad pathogens. I like products that contain multiple ingredients in a broad spectrum blend as well as biofilm busters, such as Biocidin by Bio-Botanical Research. Dosage is dependent on your health and the type/s of infection you have so I can’t go into detail about this here.
Probiotics - These are essential to help colonise the GI tract with good bacteria. It should be noted here that some individuals with SIBO who do not tolerate probiotics initially so we may delay the use of probiotics until their gut is ready to handle them. Look for a product that contains 50 billion units to help bring in some good strains of bacteria and fight off all the bad guys that are trying to take over. Take 1-2 daily with main meals and away from natural antimicrobial herbal blends.
Digestive enzymes - I start my clients on digestive enzymes to support their digestion through the pathogen eradication process. Look for brands that contain protease (breaks down protein), amylase (breaks down carbs) and lipase (breaks down fats). Have digestive enzymes with each of your main meals.
Liver Support - All of the toxins from the bugs are removed from the body via your liver. Once you start to kill them off this places a massive load on your liver so you must be taking liver support products to help with detoxing. Dosage is dependent on the product you choose and is usually taken once daily.
Additional extras for support and healing:
Mucosal Barrier support - for some individuals who have a leaky gut it is essential to support healing of their gut lining at the same time as killing off the bad bugs. Again, I like to use a mucosal barrier support herbal blend for this.
Adrenal Support - Your adrenals manage your stress hormones and while you are removing bugs your body is VERY stressed. So, we need to support your adrenals throughout this process by taking an adrenal support blend in the mornings and at lunch time.
Constipation clear-out natural options: if you are constipated, your body is storing toxins that will be making you feel terrible. This needs to be cleared and daily bowel movements must happen before you begin to cause more toxic burden on your body as the bugs die off. If you want more information about how to clear constipation, please CLICK HERE to receive my FREE Constipation Clear-out guide.
“What about antibiotics?” you say. Well, that is a topic for a whole other blog post, but let’s just say that antibiotics on their own are good at killing some bacterial gut infections in the short term (weeks) but have very poor relapse rates (because of longer lifecycles of some bugs, amongst other things) and often cause so much damage to your good gut bacteria that your risk of chronic, autoimmune and other diseases increases significantly (7, 21, 22). Not really worth it when there are other options available.
Next steps…
So, there you go - everything (and more) you need to know about gut infections! If you are interested in getting tested for a gut infection and having a personalised healing protocol developed specifically for you, please head to the Work With Us page to learn more about how we work online with clients in many countries to test for and treat the various root causes of IBS symptoms and other GI conditions.
References:
Janeway CA Jr, Travers P, Walport M, et al. (2001). Immunobiology: The Immune System in Health and Disease. 5th edition. New York: Garland Science. The mucosal immune system LINK
Smith, J. (2003). The role of gastric acid in preventing foodborne disease and how bacteria overcome acid conditions. J Food Prot. 66(7), 1292-303 LINK
Segerstrom, S. C., & Miller, G. E. (2004). Psychological Stress and the Human Immune System: A Meta-Analytic Study of 30 Years of Inquiry. Psychological Bulletin, 130(4), 601–630 LINK
Sarkar, D., Jung, M. K., & Wang, H. J. (2015). Alcohol and the Immune System. Alcohol Research : Current Reviews, 37(2), 153–155 LINK
Pietschmann, N. (2015). Food Intolerance: Immune Activation Through Diet-associated Stimuli in Chronic Disease. Altern Ther Health Med, 21(4), 42-52 LINK
Phillips, M. L. (2009). Gut Reaction: Environmental Effects on the Human Microbiota. Environmental Health Perspectives, 117(5), A198–A205 LINK
Macfarlane, S. (2014). Antibiotic treatments and microbes in the gut. Environ Microbiol, 16(4), 919-24 LINK
Josenhans. C., Suerbaum, S. (2002). The role of motility as a virulence factor in bacteria. Int J Med Microbiol, 291(8), 605-14 LINK
Popoff, M. R., & Poulain, B. (2010). Bacterial Toxins and the Nervous System: Neurotoxins and Multipotential Toxins Interacting with Neuronal Cells. Toxins,2(4), 683–737 LINK
Magge, S., & Lembo, A. (2012). Low-FODMAP Diet for Treatment of Irritable Bowel Syndrome. Gastroenterology & Hepatology, 8(11), 739–745. LINK
Calam, J., et al. (1997). How does Helicobacter pylori cause mucosal damage? Its effect on acid and gastrin physiology. Gastroenterology, 113(6 Suppl), S43-9 LINK
Ramsay, P., Carr, A. (2011). Gastric acid and digestive physiology. Surg Clin North Am, 91(5), 977-82 LINK
O’Connor, S. M., Taylor, C. E., & Hughes, J. M. (2006). Emerging Infectious Determinants of Chronic Diseases. Emerging Infectious Diseases, 12(7), 1051–1057 LINK
Carding, S., Verbeke, K., Vipond, D. T., Corfe, B. M., & Owen, L. J. (2015). Dysbiosis of the gut microbiota in disease. Microbial Ecology in Health and Disease, 26, 10.3402/mehd.v26.26191 LINK
Roberts, T., et al. (2011). Comparison of Microscopy, Culture, and Conventional Polymerase Chain Reaction for Detection of Blastocystis sp. in Clinical Stool Samples. The American Journal of Tropical Medicine and Hygiene, 84(2), 308–312 LINK
Morgan, U. M., et al. (1998). Comparison of PCR and Microscopy for Detection of Cryptosporidium parvum in Human Fecal Specimens: Clinical Trial. Journal of Clinical Microbiology, 36(4), 995–998 LINK
Choi, C. H., & Chang, S. K. (2016). Role of Small Intestinal Bacterial Overgrowth in Functional Gastrointestinal Disorders. Journal of Neurogastroenterology and Motility, 22(1), 3–5 LINK
Ford A., et al. (2009). Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol, 7(12), 1279-86 LINK
Saad, R., et al. (2014). Breath Testing for Small Intestinal Bacterial Overgrowth: Maximizing Test Accuracy. Clinical Gastroenterology and Hepatology, 12(12) 1964–1972 LINK
Prins, J. M., van Deventer, S. J., Kuijper, E. J., & Speelman, P. (1994). Clinical relevance of antibiotic-induced endotoxin release. Antimicrobial Agents and Chemotherapy, 38(6), 1211–1218. LINK
Lauritano, E., et al. (2008). Small intestinal bacterial overgrowth recurrence after antibiotic therapy. Am J Gastroenterol, 103(8), 2031-5 LINK
22. Tlaskalová-Hogenová, H., et al. (2004). Commensal bacteria (normal microflora), mucosal immunity and chronic inflammatory and autoimmune diseases. Immunol Lett, 93(2-3), 97-108 LINK