Anxiety, Depression and Gut Health: It’s Not All in Your Head
Studies have shown that as many as half of those with IBS, also suffer from psychological disorders including anxiety and depression. And while many sufferers have been told their gut symptoms are ‘all in their head’ (including me at one point), science has recently discovered the relationship might actually be the other way around. What’s happening in your gut, directly affects what’s happening in the brain, your mood and how you respond to stress.
With around 20% of the the population suffering from IBS and the World Health Organisation (WHO) identifying anxiety and depression as one of the most frequently diagnosed disorders in developed countries, this is a major breakthrough in neuroscience. And given that healing your gut is a whole lot easier than ‘healing’ your brain, it’s also a major breakthrough for anyone with IBS, who also suffers from anxiety and/or depression.
The old science and the new
It’s also important to point out that the brain can impact the gut. While scientists describe it in terms of the HPA-axis, you might have experienced it first hand as ‘nervous butterflies in the stomach’ or a ‘gut feeling’. This is something that has been known for many years. What is relatively new in the world of neuroscience is that the relationship is bidirectional. And it is the gut-to-brain direction we are going to focus on in this post.
Now, I’m no neuroscience expert and these concepts are pretty complex so bear with me. And while I don’t specialise in treating those with severe anxiety or depression, these are symptoms I see a lot of in my IBS clients. Which is why I decided to research and get up to speed on the latest science about how the two are connected and the evidence that exists for treating anxiety and depression via the paradigm of digestive health.
The gut-to-brain connection - potential mechanisms
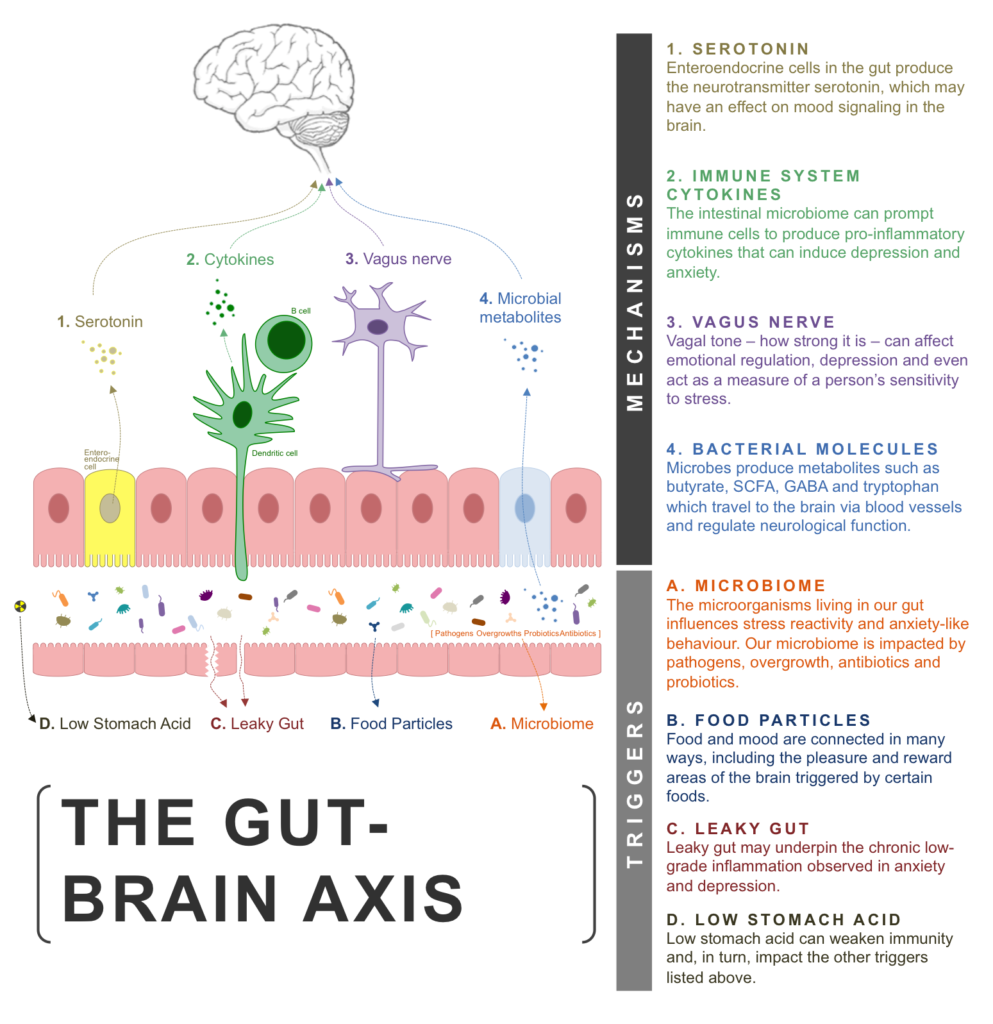
So, how does the gut affect the brain? Well, researchers think there may be four major mechanisms that make up the gut-brain-axis:
1. Serotonin - Certain cells in the gut produce the neurotransmitter serotonin, which may have an effect on mood signaling in the brain.
2. Immune system cytokines - The intestinal microbiome can prompt immune cells to produce pro-inflammatory cytokines that can induce depression and anxiety.
3. Vagus nerve - Vagal tone (how strong it is) can affect emotional regulation, depression and even act as a measure of a person’s sensitivity to stress.
4. Bacterial molecules - Microbes produce metabolites such as butyrate, SCFA, GABA and tryptophan which travel to the brain via blood vessels and regulate neurological function.
Gut Brain Axis Depression Anxiety
The triggers - what’s good (and not so good) for your gut-brain-axis
Although the science is continuously evolving, here’s what we know so far in terms of things that can trigger or mediate the mechanisms of the gut-to-brain axis listed above. It’s important to point out that these triggers are not necessarily independent of each other.
A healthy microbiome
We’ve talked about our microbiome (gut flora) before. Studies have demonstrated that the collection of microorganisms living in our gut influences stress reactivity and anxiety-like behaviour. Recent research examined the composition of gut bacteria in patients with depression compared to healthy individuals and reported significant differences with increased population of Bacteroidetes, Proteobacteria, and Actinobacteria, and decreased population of Firmicutes in patients with depression.
So while it is likely to be a lot more complicated than the existence or otherwise of specific strains of bacteria, having a large abundance and diversity of good gut bacteria is almost certainly key to maintaining superior brain health.
Pathogens
Pathogens are the bad guys - things like specific strains of overgrown yeast, bacteria and parasites that shouldn’t be living in our gut. It is now accepted that gut infections can cause anxiety, depression and cognitive dysfunction. It was actually a long term study on a Giardia (parasite) outbreak in Norway that helped make the possible connection between gut bacteria and psychological conditions in the first place.
More directly, Campylobacter jejuni, a pretty common gut bacteria in those with IBS symptoms, given to rats in small doses led to anxiety-like behavior without a detectable immune response. The inference being that even if you don’t have IBS symptoms, your anxiety could still be caused by a low-grade gut infection like Campylobacter.
The mechanism is thought to involve cytokines, the vagus nerve and bacterial molecules, highlighting that very often no one mechanism is working alone within the gut-brain axis.
Antibiotics
The life-saving benefits of antibiotics do, unfortunately, come with side-effects. And one of the lesser known side-effects is to do with psychological and mood disorders like anxiety and depression. A particularly well known, large scale eighteen-year case-controlled study, recently found that even a single antibiotic course was associated with higher risk for depression, with recurrent antibiotic use increasing the risk further.
This is not surprising, given what we know about the importance of a healthy and diverse microbiome to our mood and brain health and the negative impact antibiotics have on our beneficial gut flora. The association between increasing overprescription of antibiotics and the rise in prevalence of deteriorating gut health, it’s unlikely just a coincidence.
Probiotics (Psychobiotics)
Although the focus on our microbiome and probiotics for treating anxiety and depression seems to only be a recent development, the first documented probiotic treatment for depression was implemented in 1910.
Scientists are now referring to some probiotic strains as psychobiotics because of their ability to influence brain and mood function. Here’s just a few of the recent studies done on probiotics and depression and anxiety:
> A meta-analysis of five randomised controlled trials completed in the last decade found that ‘probiotics were associated with a significant reduction in depression, underscoring the need for additional research on this potential preventive strategy for depression’.
> Lactobacillus and Bifidobacterium probiotic formulation taken in combination significantly reduced anxiety-like behaviour in rats and alleviated psychological distress in healthy human volunteers - study.
> Regularly eating yogurt with probiotics, which contain “good” bacteria, positively affects brain functioning related to emotions in women - study.
> Elevated stress response and depression in rats was reversed by administering a single bacterium, Bifidobacterium infantis - study.
> Rats given Lactobacillus rhamnosus probiotics for 28 days showed a decline in both anxiety and depression scores. This is thought to be a result of regulation of bacterial molecule (GABA) receptors via the vagus nerve - study.
Small Intestinal Bacterial Overgrowth (SIBO)
SIBO is the result of an overgrowth of bacteria or archaea in the small intestine. These bacteria ferment carbohydrates in the small intestine causing increased gas production. This fermentation also produces short-chain fatty acids (SCFA) such as butyrate, acetate, and propionate.
This is important because SCFAs, produced by the bacterial fermentation of dietary carbohydrates, regulate the immune system and can cross the blood-brain-barrier, affecting brain development and behaviour. It is not surprising then that in some studies, eradication of SIBO has been shown to improve symptoms of depression.
Food
Food and mood are connected in many different ways. Overeating and obesity is often associated with depression and anxiety, although this may have less to do directly with the food we eat and more to do with our microbiome. That is, the same balance of gut bacteria that makes you fat might also make you anxious or depressed.
More commonly understood is the way in which we use certain ‘comfort’ foods to try and regulate our mood and the effect of certain foods on pleasure and reward regions of the brain.
Intestinal Permeability (Leaky Gut)
According to recent scientific findings, increased intestinal permeability may underpin the chronic low-grade inflammation observed in disorders such as depression and may have further negative effects on mood, anxiety, cognition and social interaction. Studies on rodents have shown how intestinal hyper-permeability (‘leaky gut’) can increase the production of inflammatory cytokines as bacteria enter the bloodstream through the walls of the GI tract.
Reflux and Low Stomach Acid
Hydrochloric acid (HCl) produced in the stomach is essential for killing bacteria, fungi and parasites that come in on our food and water, and for the digestion of protein and minerals. Low levels can weaken immunity and, in turn, lead to many of the problems listed above including the inability to break down foods and kill gut infections before they can enter the GI tract. This may be why studies have found a connection between those with depression and reflux conditions like GERD.
In summary
Anxiety, depression and other psychological and mood disorders are complex conditions with a variety of root causes that differ from client to client. Not everyone who suffers from anxiety or depression is going to have their symptoms improve completely through healing the gut.
But, for those with IBS-type symptoms, it can be a relief to know that this might be the case for you. I’ve seen enough client’s anxiety and depression lifted and the need for antidepressant medication removed to know that healing the gut should be the first place you look.