Natural SIBO Treatment Protocols: 2024 Guide
SIBO (Small Intestinal Bacterial Overgrowth) is infamously difficult to kill and even more difficult to keep that way. This is because attacking a small intestinal bacterial overgrowth with anything less than a really comprehensive natural treatment protocol, that is more than just diet or antibiotics, is essential for long-term healing. Natural SIBO treatment protocols that rely on single herbal products just don’t seem to cut it. And secondly, because SIBO is often the consequence of some other dysfunction or imbalance within the body, if this is not resolved alongside SIBO eradication, it can increase your risk of relapse and the need for further SIBO treatment. Layer over the top of these challenges the huge variety of symptoms seen amongst SIBO sufferers, which means that intervention needs to be tailored specifically to the individual, and you start to understand why natural SIBO treatment really is the domain of practitioners specializing in this condition.
With that in mind, we wrote this blog post series originally back in 2016 and have been constantly updating it to help you understand the latest research and intervention options available. The science of natural SIBO treatment is ever-changing as new research sheds light on the most effective options we have around. This basically means that what we do today is completely different to what I was doing (and what you might read on old blog posts and forums) to treat SIBO three or four years ago. So, where to start with the most cutting edge, all natural SIBO treatment and herbal options? We’ve divided this ‘treatment’ approach post up into the four phases we use with our SIBO clients.
Here is a summary of what we are going to cover in Part 3:
> How to make changes to your diet that reduce your SIBO symptoms fast
> The three most effective ways to remove a SIBO overgrowth
> Natural herbal SIBO treatment considerations for an effective SIBO protocol
> Why supporting digestion and detoxification while eradicating SIBO is essential
> When to introduce prebiotics and probiotics for SIBO and how to avoid aggravating your symptoms
> The importance of addressing the root cause of SIBO and why relapse is so common
> Access to our Fullscript Dispensary and 20% Off SIBO supplements
Refresh on SIBO symptoms and SIBO testing
SIBO Symptoms
If you’re looking for a recap on the basics of SIBO, read this post: Is SIBO The Hidden Cause of Your IBS?
> What is SIBO and how it can ruin your health
> Why it’s important to know which ‘type’ of SIBO you have
> Symptoms to look out for and why SIBO is often the cause of IBS
> The most common underlying root causes of SIBO?
SIBO Testing
If you’re looking for a recap on SIBO testing, read this post: The Science (and Art) of SIBO Testing
> The ‘gold-standard’ SIBO test you need to ask your practitioner about
> Why a negative test result doesn’t always mean you don’t have SIBO
> Why SIBO testing and SIBO retesting is so important
> Other GI testing you should consider
Natural SIBO Protocol Approach
Here is an diagram overview of our approach to SIBO treatment using a comprehensive and holistic approach which will discuss throughout this article:
PHASE 1: REDUCE SIBO SYMPTOMS USING DIET
If you have raging SIBO symptoms and/or have just received a positive SIBO diagnosis, the very first thing you want to do is get your symptoms under control. The fastest way to do this is through diet. And while diet is a great short-term symptom management tool, it’s important to keep in mind that diet alone will not heal a bacterial overgrowth in the small intestine. Starving the bacteria of their fuel source helps, but if you continue with such a restricted diet for a long period of time, you also risk starving the beneficial gut bacteria in your large intestine (your microbiome) that play a vital role in your health and that help keep SIBO at bay (1, 2).
Feed the bacteria or starve them?
Let’s get into some of the SIBO diet options you might have heard about so you can understand how they work. There are two distinct theories about how to approach SIBO treatment so we will mention them both.
Feed to kill. The first approach is to actually eat fermentable carbohydrates during treatment to feed the overgrown bacteria. While you are more likely to experience symptoms while consuming fermentable carbohydrates, this approach is based on the assumption that happy and well-fed overgrown bacteria are more sensitive to antimicrobials and are easier to kill. Alternatively, when starved, bacteria go into a sort of ‘survival mode’ where they do not replicate and are therefore harder to penetrate with antimicrobials (3). The ‘feed the bacteria’ approach may work better if you are opting for a short-course of antibiotics (7-14 days), but will be less tolerated on 30-60 days of natural antimicrobials because most people don’t want to exacerbate their symptoms for that long.
Starve with restricted diets. Bacteria predominantly feed off carbohydrates, and particularly enjoy fermentable carbohydrates. By using restricted diets that limit these carbohydrates, we can reduce the overgrown bacteria’s food source, and limit SIBO symptoms. While it’s easy to become reliant on these restricted diets for symptom management, they generally won’t eradicate SIBO on their own and can actually have long-term negative impacts on our gut microbiome if followed for too long. You can learn more by reading our blog post on this specific topic: 5 signs you’ve been on an IBS elimination diet for too long
Our approach to SIBO diets
Our clinical approach to diet in both this initial phase, and during phase two, is to focus on reducing symptoms caused by the bacterial overgrowth. We do this by reducing the main food source that the overgrowth feeds on - fermentable carbohydrates.
This means that certain carbs in your diet are going to cause some level of bloating, gas, diarrhoea or constipation, etc, if you have SIBO. These include:
> Starch - grains, beans, high starch vegetables
> Resistant starch - whole grains, seeds, legumes
> Soluble fibre - grains, beans, nuts, seeds, vegetables, fruit
> Sugar - fruit, dairy, sweeteners
> Prebiotics - beans, vegetables, roots, herbs, prebiotic supplements
Proteins and fats are your friend at this point and make up the majority of the diet designed to limit SIBO symptoms. Two diet options that are low in fermentable carbohydrates that we like to use with our clients are SCD/low-FODMAP and Paleo/low-FODMAP. For those who are very sensitive to oxalates, histamines, amines, salicylates, sulphur or other food components, or who have food sensitivities, we will layer this over the top, however sometimes you have to compromise with these otherwise there would be (almost) no foods left to eat.
Diet is very individual and you can achieve dramatic improvements in symptoms in a short time-period if you figure out what works best for you. We should also make a note here that this type of diet seems to work equally well for the hydrogen-producing bacteria type of SIBO as it does for the methane-producing archaea type of SIBO. This is because as you stop over-feeding the hydrogen-producing bacteria by limiting specific carbs, you are also limiting the hydrogen gas used as fuel by the archaea to produce methane.
Tips to reduce inflammation and promote gut healing
Another thing to note about the diets we use is that by limiting carbohydrates, we are also limiting inflammation-causing anti-nutrients that are commonly found in grains, legumes, nuts and seeds. While normally tolerated, these foods can be problematic for anyone with a compromised digestive system. By avoiding them in the short-term, we are also helping to reduce gut inflammation. Here are a few tips we give our clients starting Phase 1:
> Aim for 70% cooked and 30% raw foods. Cooking vegetables and fruit will lower the fibre and resistant starch content making them less likely to cause you symptoms.
> Ensure fruit is ripe, as under-ripe fruit is high in resistant starch which can cause symptoms.
> Limit snacking between meals (4-5 hours) to give the migrating motor complex (MMC) a chance to move bacteria and food remnants from the small intestine to the large intestine ready for excretion from the body.
> There are other food sources such as alcohol, caffeine and artificial sweeteners that can compromise healing by providing fuel for the bacterial overgrowth. This is why we ask our clients to limit them during SIBO treatment.
> Fermented foods; at this stage of healing, we ask our clients to limit fermented foods like sauerkraut, kombucha, kefir, etc, as they generally aggravate symptoms.
PHASE 2 (PART A): REMOVE THE OVERGROWTH
With diet keeping symptoms under control, the next step is to remove the overgrowth. There are three main options here; natural antimicrobials, antibiotics and the elemental diet. Because of SIBO’s notorious stubbornness, for many clients their treatment will involve a combination of two or even three of these approaches over successive protocols. Each has its strengths and weaknesses and are more or less suited to different clients - there is no one ‘magic SIBO protocol’ for all SIBO cases. With that in mind, we’ll discuss each one in the order they are most commonly used.
Natural herbal antimicrobials for SIBO - preferred SIBO treatment approach
My preferred approach involves all-natural eradication protocols using natural herbal antimicrobial supplements for SIBO. Not only do we find them less aggressive, they have also been shown to be at least as effective as antibiotics in clinical trials (4). Two important principles to keep in mind with antimicrobials for a SIBO protocol are:
1) Combine to kill - there are varying types of bacteria and archaea that can cause SIBO and not all antimicrobials can kill off all types. The best way to overcome this is to combine single-ingredient products or use blends for maximum effectiveness.
2) Rotate to avoid resistance - bacteria are smart and will adapt quite quickly. While not as common as antibiotic resistance, the effectiveness of a given herb tends to diminish with successive rounds of use.
Most SIBO protocols last around 30-45 days per cycle (most clients need to complete multiple cycles, depending on their levels of bacterial overgrowth) and vary by the type of SIBO you have. As a general rule for:
- Hydrogen-dominant SIBO we like to use berberine with neem or oil of oregano
- Methane-dominant SIBO we like to use allicin with oil of oregano or neem.
In terms of specific products we often use with clients (available on our Fullscript Dispensary):
> Allicin (Garlic) - Allimax Nutraceuticals, Allimed Capsules 450mg.
> Oregano - Biotics Research, A.D.P. Oregano.
> Neem - Ayush Herbs, Neem Plus.
> Berberine - Integrative Therapeutics, Berberine Complex
Other great herbs for SIBO to consider are cinnamon, thyme and pomegranate which also work really well for those with Candida or Blastocystis hominis. You can access some great SIBO supplement blends such as Candibactin AR and BR and Biocidin that have multiple herbs in them. We like to use these when a client has parasites, bacteria or yeast in their large intestine, in addition to SIBO.
Another benefit of using antimicrobial supplements for SIBO protocols is that we can use blends that address other issues indirectly, such as hydrogen sulfide SIBO and SIFO (Small Intestinal Fungal Overgrowth), a very common comorbidity for SIBO sufferers, affecting around half of SIBO cases (5).
You can access these (and many more) products from our Fullscript Dispensary at 20% OFF RRP. You will need to sign-up to create a Fullscript account to access these products and discounts and find them in our favorites under ‘SIBO Antimicrobials’. Click the link below or visit: https://us.fullscript.com/welcome/blindemann
Where do conventional antibiotics for SIBO fit in?
Antibiotic SIBO treatment protocols have evolved substantially over the last decade and now offer a second line treatment or alternative to natural antimicrobials for SIBO. A move away from broad-spectrum antibiotics to variations that are non-absorbable and small intestine-specific have increased effectiveness and reduced systemic side effects, such as urinary tract infections and the development of leaky gut and food sensitivities.
Rifaximin (Xifaxan) is currently the most commonly used antibiotic for SIBO treatment and has reported success rates of around 50% for those with hydrogen-dominant SIBO (6). While less effective for methane-dominant SIBO, one study has reported success rates as high as 85% using a combination of Rifaximin and another antibiotic called Neomycin (7). Relapse rates of around 50% at nine months (8) mean that even after initially successful treatment, it’s important to be vigilant with symptoms, heal the gut and focus on fixing the underlying root cause (phases 3 and 4). Because of issues with resistance after repeated rounds (9) and for those not able to clear SIBO with antibiotics, natural antimicrobials have reported clearance rates over 50% in those who fail on Rifaximin (4).
SIBO Elemental Diet - when all else fails
For clients who have completed multiple rounds of antimicrobials (or antibiotics) without success, the SIBO Elemental Diet is another standalone option available with strong clinical evidence (10). It basically involves drinking powdered, predigested nutrients that are mixed with water and removing all solid foods from your diet for 2-3 weeks. Because the nutrients in this form are absorbed so rapidly, the bacteria do not have a chance to feed on them and use them as fuel. The idea is to completely starve the bacteria of nutrients in a more extreme way to an SCD + low-FODMAP style diet.
I like to use the SIBO elemental diet as a last-resort option as avoiding real food isn’t exactly natural and often more than two weeks is required. It can be challenging due to the taste, removal of all solid food and ability to be social around mealtimes, as well as SIBO die-off symptoms potentially being more severe compared to when you are treating using herbal antibiotics.
The product we currently use is Physicians’ Elemental Diet Dextrose Free by Integrative Therapeutics, which contains a balanced blend of macronutrients, essential vitamins, minerals, and electrolytes to act as a sole source of nutritional intake for a two to three week period. However, given that each large bag only provides 3-4 days worth of meals (depending on your caloric needs), it can get quite expensive if you aren’t getting it at discounted prices through a practitioner - you can find it on our Fullscript Dispensary at 20% OFF RRP: https://us.fullscript.com/welcome/blindemann
Treating SIBO Biofilm
An estimated 75% of bacterial infections, and possibly higher in archaeal and fungal infections, involve biofilms (11, 12, 13). Biofilms are colonies of microorganisms that are protected by an extracellular matrix - which we think of simplistically as a protective home for the infection to live in. This protective home makes the infection up to 1000 times more resistant to antibiotic therapies and therefore, more difficult to kill (11, 14). This is why a SIBO biofilm disruptor should be considered in a comprehensive treatment protocol.
Busting up the biofilm whilst using antimicrobials can be achieved by incorporating specific herbal products. We like to use blends such as Biofilm Defence by Kirkman Labs, InterPhase Plus by Klaire Labs or Biofilm Phase-2 Advanced by Priority One as all are well tolerated by our clients and contain the right ingredients to break down biofilms (available on our Fullscript Dispensary).
To learn more about Biofilms and how to address them in your protocols, read our Biofilm Treatment Protocol blog.
PHASE 2 (PART B): SUPPORTING DIGESTION AND DETOXIFICATION
Digestion support considerations
Whilst taking antimicrobials during this phase, it is also important to support digestion and absorption of the nutrients you eat. We do this because an overgrowth in the small intestine will block the intestinal lining where absorption of the nutrients in the foods we eat happens (15). This means taking supplements like digestive enzymes that help you break down and absorb the foods you eat; stomach acid support from betaine HCL to help with killing off any bad bacteria that is contaminating the foods you eat, which also assists with protein and fat digestion; and nutritional support in the form of anti-inflammatory fish oil capsules and multi-minerals supplements if needed.
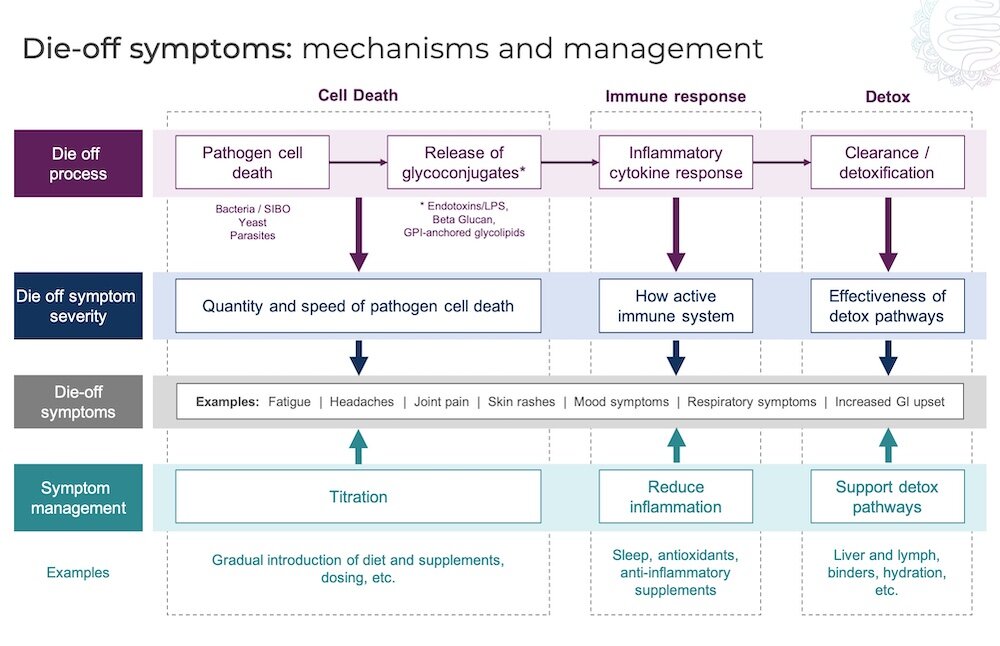
Detoxing is a MUST
The next thing we need to focus on in this phase is supporting the body with detoxification. During die-off of the bacterial overgrowth, there is often a buildup of toxins in the body that needs to be removed. This places excess stress on the liver, our main detoxification organ, so we have our clients support their liver using a herbal blend supplement. We also ask them to use a charcoal and bentonite clay product for a few days each week, when they are actively killing off the overgrowth, to help with removal of the toxins and debris from the gastrointestinal tract. We’ve written a whole blog post on Die-Off Symptoms and Managing Detox HERE.
Constipation and toxicity
Constipation, which is a very debilitating symptom for those with methane-producing archaea, must be dealt with as an absolute priority (16). If there is especially-toxic bacteria and archaea-filled waste being stored in the colon for extended periods of time, the body can reabsorb these toxins. This is particularly important for those who experience more severe SIBO die-off symptoms. We must keep the colon clear so we encourage clients to take a poorly absorbed form of magnesium (such as magnesium citrate or oxide) and vitamin C daily, as well as complete a vitamin C flush weekly where constipation is severe. If you want more information about how to clear constipation, please CLICK HERE to receive our FREE Constipation Clear-out eguide.
Finally, at the end of each round of antimicrobials or after completing the elemental diet, it is essential that we re-test.
PHASE 3 - REPOPULATE THE GOOD BACTERIA & HEAL THE GUT LINING
With the SIBO overgrowth eradicated, the focus shifts to repopulating the gut with the right balance of flora and healing the gut lining to support long term health and prevent a relapse.
Probiotics for SIBO - yes or no?
Unfortunately, it’s much more complicated than that. It’s about what type of SIBO you have, with your symptoms and client history, which strains of probiotics you have tried, how much and at what point in your SIBO treatment to introduce them. It is also important to take into consideration how well you tolerate histamines, since histamine-degrading enzymes are located in the small intestine and often impacted by SIBO. It is one of the many reasons that DIY treatment and off-the-shelf protocols don’t often work for SIBO sufferers… there are just too many variables and a constant need to review and refine a personalized approach.
While not all clinicians agree, the science published so far is pretty clear; probiotic supplements are an effective SIBO treatment both as a stand alone (17) and as a follow-up to SIBO herbal antibiotics (6). The three most beneficial strains of SIBO probiotics to look out for are bifidus infantis, bifidus lactis, and lactobacillus plantarum. These can be taken individually, or in combination. As with all supplements, titrate (introduce) them slowly and build up to a level that you tolerate. More is not always best when supporting the natural population of bacteria in the small intestine.
An alternative school of thought is a concern with adding bacteria in the form of SIBO probiotic supplements to an overgrowth of bacteria that’s already there. And there are some clients whose symptoms are obviously aggravated by SIBO probiotic supplements. For these clients, it can be a bit of (frustrating) trial and error - you may need to try different strains or combinations to find the one that works for you. But in our experience, probiotics are not a make or break part of natural SIBO treatment and for clients who do not tolerate probiotic supplements during eradication, we usually focus on introducing them in this phase.
After SIBO treatment is finished, we titrate the above mentioned strains in supplement form at a very gradual pace. This often means breaking open a capsule and sprinkling out a small amount before building up to more standard dosages.
A note of caution: it’s probably best to avoid your general store bought probiotics for SIBO as many of them contain ingredients that will aggravate your symptoms, including; D-lactate-forming species like Lactobacillus acidophilus, or tapioca and potato starch, maltodextrin, lactose, inulin, pectin as well as other prebiotics that may cause issues.
Probiotic rich foods are another way to help repopulate the gut microbiome and improve the balance of flora in the small intestine. As with probiotic supplements, we tend to move slowly with these foods and usually after successful eradication in phase two. We like to start clients on small amounts of coconut kefir, before building up to fermented vegetables like sauerkraut, if tolerated. Food like kimchi, miso and tempeh are a few examples of fermented foods that we use with our clients, and that are gaining popularity in the health community.
Are prebiotics the new probiotics for SIBO?
The story with prebiotics is pretty similar to that of probiotics for SIBO. Prebiotics are actually the fuel that feeds bacteria. This means if you still have an overgrowth, generally most prebiotics will aggravate symptoms. Raw chicory root, Jerusalem artichoke, dandelion greens, leeks, garlic and onion are all examples of prebiotic-rich foods that are best avoided.
However, feeding the good guys and encouraging the right balance of flora is an important part of the long-term healing journey. There is obviously a delicate balance here and prebiotics are something that needs to be introduced slowly. We have found clinically that introducing specific prebiotics, like Partially hydrolyzed guar gum (PHGG), during the elimination phase and only when tolerated, can actually have a positive impact on symptoms and elimination of SIBO.
As with many complicated conditions, there are clients who seem to thrive on prebiotics during and after natural SIBO treatment, something that is not yet well understood but will hopefully become clearer over time. It just highlights the point that what works for some people, will make things worse for others (and visa versa).
The importance of healing the gut lining after natural SIBO treatment
Another important role of prebiotics and probiotics in this phase is with healing a leaky gut, which has most likely developed as a result of SIBO (18). By replenishing the beneficial bacteria in the small intestine, prebiotics and probiotics can reduce overgrown or harmful bacteria, inhibit yeast overgrowth, improve motility and reduce inflammation, all of which are important for gut healing (19). Restoring the health of the small intestine and the gut lining is critical to reducing the risk of a SIBO relapse.
While there are additional supplement and diet recommendations available for healing a leaky gut, there is a lot of overlap between SIBO and leaky gut protocols. Most clients see significant improvement simply by removing the SIBO, along with the continuation of a maintenance diet and supplement protocol for up to 6 months post SIBO treatment.
PHASE 4 - REPAIR BY ADDRESSING THE UNDERLYING ROOT CAUSE TO AVOID SIBO RELAPSE
Despite being mentioned last, this phase is probably the most important of all and actually begins right at the start of any elimination strategy; address the possible root causes of your SIBO so it doesn’t come back again. Sadly, SIBO is strongly associated with chronic relapse (15), largely because 1) killing off the overgrown bacteria (or archaea) can be difficult; and 2) killing the bacteria itself doesn’t necessarily fix the root cause of why you have the SIBO to begin with. Whether that is a poorly functioning migrating motor complex (most common), a structural issue like adhesions or an open ileocecal valve, a functional issue like hypochlorhydria, immunodeficiency, altered bile flow or enzyme production, or even previous mold exposure, root causes need to be investigated and addressed.
Healing the migrating motor complex
The most common cause of SIBO is an impaired migrating motor complex (MMC), as discussed in part 1 of this blog series. The migrating motor complex is a wave of movement, that happens every 90 to 120 minutes in the stomach and small intestine, moving bacteria and undigested material down into the large intestine during fasting at night and between meals (20). Sadly, bacteria can overgrow again within two weeks of finishing treatment if the migrating motor complex is not working effectively. As such, a post-treatment natural prokinetic needs to be used to stimulate the migrating motor complex and keep things moving (21).
Prokinetics are typically started around the completion of antimicrobials and ideally when the retest result is clear. The purpose of using a natural prokinetic for SIBO is to reset the migrating motor complex. Failure to use an effective natural prokinetic is one of the most common reasons for relapse amongst SIBO sufferers. Additionally, it is important that you stay on a prokinetic for a minimum of 6 months after SIBO treatment, even if symptoms have completely resolved. There are a few great options for natural prokinetics, including Iberogast; Pure Encapsulations, Motilpro; Integrative Therapeutics, Motility Activator; Priority One, SIBO-MMC; ginger root and many more (available on our Fullscript Dispensary)
Other structural and functional healing
Beyond the migrating motor complex, there are a vast array of potential underlying root causes of recurring SIBO overgrowths, specific to each individual. Depending on your medical history, comorbidities and current lifestyle, your practitioner should be able to work through solutions to any remaining imbalances that could increase your risk of relapse. They include boosting stomach acid production, avoiding excessive exercise, reducing stress and addressing structural issues like ileocecal valve dysfunction and adhesions.
Maintenance - SIBO relapse prevention
With SIBO relapse rates commonly reported up to a year after eradication, the maintenance phase should last between 6 - 12 months after completing natural herbal antimicrobials for SIBO and a retest without any elevations in hydrogen or methane gas.
If you find that your symptoms continue or return, you might need to retest or consider testing for and address mold, parasites, bacteria or yeast in the large intestine, SIFO, or ongoing inflammation from food sensitivities. Remember, symptoms are a sign that there is an underlying imbalance in systems of the body that need to be healed (not ignored).
Natural SIBO treatment protocol summary
The science of herbal natural SIBO treatment and testing are continuing to progress as evidence is constantly being added to the growing body of research. This means that what we do today to heal SIBO will probably be different to what we are doing in five years time.
I honestly hope that this three-part series has helped you understand SIBO a little better, and has given you the confidence to seek out testing if you feel like it might be something that is affecting you. Healing SIBO is a journey. If you are ready to begin yours, please head to the Work With Us page to learn more about how we work online with clients in many countries to treat SIBO and other root causes of IBS symptoms.
References:
Heiman, M. L., & Greenway, F. L. (2016). A healthy gastrointestinal microbiome is dependent on dietary diversity. Molecular Metabolism, 5(5), 317–320
Halmos E., et al. (2015). Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut, 64(1), 93-100
Bryk, R., et al. (2008). Selective Killing of Nonreplicating Mycobacteria. Cell Host & Microbe, 3(3), 137–145
Chedid, V., et al. (2014). Herbal Therapy Is Equivalent to Rifaximin for the Treatment of Small Intestinal Bacterial Overgrowth. Global Advances in Health and Medicine, 3(3), 16–24
Jacobs, C., et al. (2013). Dysmotility and proton pump inhibitor use are independent risk factors for small intestinal bacterial and/or fungal overgrowth. Aliment Pharmacol Ther, 37(11), 1103-11
Peralta, S., et al. (2009). Small intestine bacterial overgrowth and irritable bowel syndrome-related symptoms: Experience with Rifaximin. World Journal of Gastroenterology : WJG, 15(21), 2628–2631
Low, K., et al. (2010). A combination of rifaximin and neomycin is most effective in treating irritable bowel syndrome patients with methane on lactulose breath test. J Clin Gastroenterol, 44(8), 547-50
Lauritano, E., et al. (2008). Small intestinal bacterial overgrowth recurrence after antibiotic therapy. Am J Gastroenterol, 103(8), 2031-5
Basseri, R. J., Weitsman, S., Barlow, G. M., & Pimentel, M. (2011). Antibiotics for the Treatment of Irritable Bowel Syndrome. Gastroenterology & Hepatology, 7(7), 455–493
Pimentel, M., et al. (2004). A 14-day elemental diet is highly effective in normalizing the lactulose breath test. Dig Dis Sci, 49(1), 73-7
Potera, C. (2010). ANTIBIOTIC RESISTANCE: Biofilm Dispersing Agent Rejuvenates Older Antibiotics. Environmental Health Perspectives, 118(7), A288
Taff, H., et al. (2013). Mechanisms of Candida biofilm drug resistance. Future Microbiol, 8(10), 1325-37
Bang, C., et al. (2014). Biofilm formation of mucosa-associated methanoarchaeal strains. Frontiers in Microbiology, 5, 353
Ramage, G., Saville, S., Thomas, D., & López-Ribot, J. (2005). Candida Biofilms: an Update . Eukaryotic Cell, 4(4), 633–638
Bures, J., et al. (2010). Small intestinal bacterial overgrowth syndrome. World Journal of Gastroenterology : WJG, 16(24), 2978–2990
Triantafyllou, K., Chang, C., Pimentel, M. (2013). Methanogens, methane and gastrointestinal motility. J Neurogastroenterol Motil, 20(1), 31-40
Soifer, L., Peralta, D., Dima, G., Besasso, H. (2010). Comparative clinical efficacy of a probiotic vs. an antibiotic in the treatment of patients with intestinal bacterial overgrowth and chronic abdominal functional distension: a pilot study. Acta Gastroenterol Latinoam, 40(4), 323-7
Riordan, S. (1997). Luminal bacteria and small-intestinal permeability. Scand J Gastroenterol, 32(6), 556-63
Aragon, G., Graham, D., Borum, M., & Doman, B. (2010). Probiotic Therapy for Irritable Bowel Syndrome. Gastroenterology & Hepatology, 6(1), 39–44
Dukowicz, A. C., Lacy, B. E., & Levine, G. M. (2007). Small Intestinal Bacterial Overgrowth: A Comprehensive Review. Gastroenterology & Hepatology, 3(2), 112–122
Pimentel, M., et al. (2009). Low-Dose Nocturnal Tegaserod or Erythromycin Delays Symptom Recurrence After Treatment of Irritable Bowel Syndrome Based on Presumed Bacterial Overgrowth. Gastroenterology & Hepatology, 5(6), 435–442
About author: Bella Lindemann, FDN-P
Bella Lindemann is the founder and lead practitioner of The Functional Gut Health Clinic. With her science degree, functional nutrition certification and extensive experience, she is a recognised expert in gut health and the science of SIBO. Having worked with hundreds of SIBO cases, including her own, she is passionate about helping her clients address this imbalance and take back control of their digestive symptoms.